Pregnancy-related deaths remain a pressing public health issue in the United States, where more than 80 percent of these fatalities are deemed preventable. With the nation boasting the highest maternal mortality rate among high-income countries, alarming trends have persisted, particularly between 2018 and 2022. Disparities based on race and geographic location further complicate these statistics, highlighting significant racial disparities in maternal health care. Key contributors to pregnancy-related deaths include cardiovascular disease, which now dominates as the leading cause during and after pregnancy. Addressing the high rates of maternal mortality requires urgent improvements in prenatal and postpartum care, targeting systemic inequalities to ensure that every woman receives the quality health care she deserves.
The alarming rise in fatalities during pregnancy, often referred to as maternal mortality, has surfaced as a critical concern in the U.S. This term encapsulates the tragic deaths of women related to pregnancy complications, many of which are preventable with proper health interventions. Significant attention must be directed toward addressing the underlying factors, including disparities in maternal health, especially among racial and ethnic groups. Furthermore, the transition of leading causes from hemorrhage to cardiovascular issues during and post-pregnancy underscores the need for innovative approaches in health care systems. As the conversation around postpartum care improvements gains momentum, it is essential to prioritize research and funding to combat this growing crisis.
Understanding the Rise in U.S. Pregnancy-Related Deaths
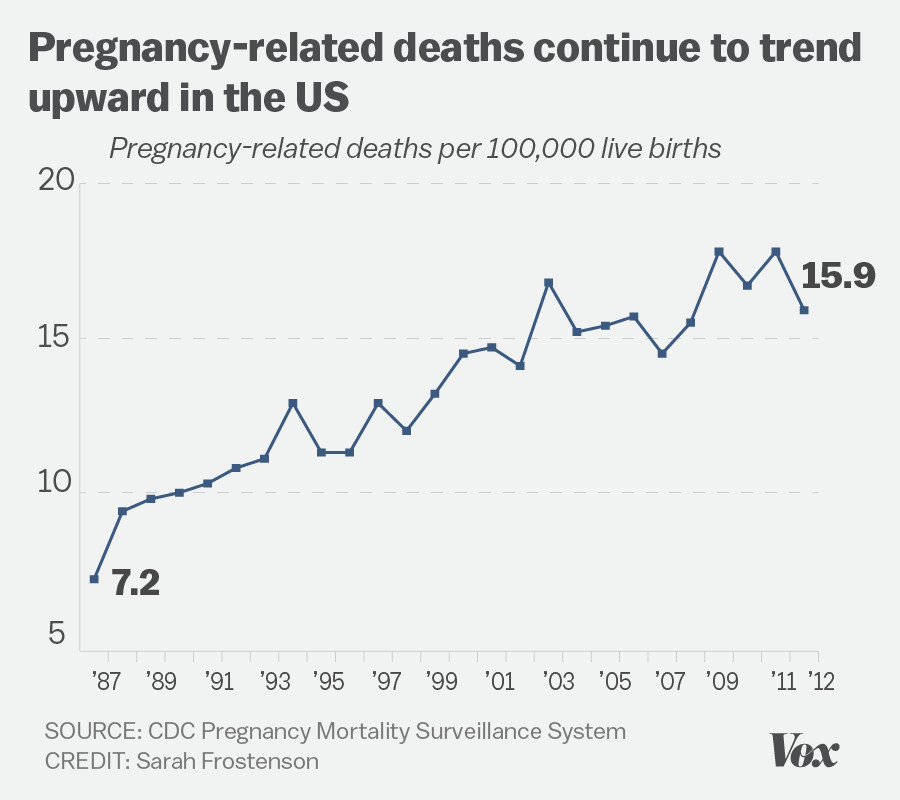
The increase in pregnancy-related deaths in the United States has raised urgent alarms, particularly as more than 80 percent of these deaths are deemed preventable. Research indicates that between 2018 and 2022, the maternal mortality rate has increased, notably influenced by the effects of the COVID-19 pandemic, which highlighted weaknesses in our healthcare system. The United States, as a high-income nation, bears the dubious distinction of having the highest maternal mortality rate, which underscores the pressing need for comprehensive measures aimed at improving prenatal and extended postpartum care.
The wide racial disparities in maternal mortality further complicate the issue. American Indian and Alaska Native women face pregnancy-related deaths at rates nearly four times higher than their white counterparts. These disparities are indicative of systemic inequities within healthcare access and quality. Without targeted intervention and policy reforms that address these discrepancies, the journey towards reducing pregnancy-related deaths remains fraught with challenges.
Research has demonstrated that chronic conditions like cardiovascular disease are increasingly linked to pregnancy-related deaths in younger women, particularly those aged 25 to 39. The persistence of chronic diseases in reproductive-age individuals underscores a critical area for intervention as we work towards addressing maternal health concerns comprehensively. By prioritizing maternal health education and preventive care strategies in younger populations, we can hopefully turn the tide on these alarming statistics.
Efforts to enhance postpartum care and address late maternal deaths—those occurring up to a year after delivery—are also crucial. Traditionally, the maternal mortality definition has ignored this broader timeline, but recent studies advocate for a more inclusive view of maternal health that encompasses long-term recovery. Understanding and improving care during this critical year can significantly reduce postpartum complications and subsequent mortality.
Preventing Pregnancy-Related Deaths: Policy and Practice Solutions
To effectively tackle the issue of preventable pregnancy-related deaths, it is imperative to reform policies focused on healthcare access, particularly in states that show the highest mortality rates. Research suggests that a modeled approach, analyzing successful systems such as California’s, could potentially reduce national mortality rates significantly. Strategies could include improved access to quality prenatal care and a focus on eliminating maternity care deserts, bridging gaps that often lead to health disparities.
Investment in public health infrastructure is another critical area that requires attention. Cuts to research funding and maternal health initiatives threaten progress, as the need for innovative solutions is more pressing than ever. Adequately funding maternal health research could provide valuable insights into effective care practices and help establish comprehensive support systems for individuals during pregnancy and the postpartum period, fostering improved outcomes across communities.
Engaging healthcare providers in continual education around the signs and risks associated with pregnancy complications, particularly chronic conditions such as hypertension and cardiovascular disease, can promote early intervention. By equipping healthcare professionals with the knowledge and tools needed to address these critical areas, we enhance the likelihood of identifying at-risk patients who would benefit from tailored care plans.
The collaboration across different healthcare sectors, including public health officials, maternal health advocates, and policymakers, is crucial in revitalizing efforts to enhance maternal health outcomes. Only through coordinated initiatives can we initiate necessary policy changes that emphasize preventive care and the importance of regular follow-ups during and well into the postpartum period, ensuring that mothers remain healthy long after childbirth.
Addressing Racial Disparities in Maternal Health
Racial disparities in maternal health outcomes highlight systemic injustices within healthcare that disproportionately affect women of color. The data revealing stark differences in maternal mortality rates between different racial groups emphasizes the need for focused intervention strategies. The rates at which American Indian, Alaska Native, and non-Hispanic Black women experience pregnancy-related deaths signal urgent public health failures that demand scrutiny and reform.
Effective strategies to address these disparities should include community-based support initiatives that empower local organizations to advocate for better healthcare access. Additionally, culturally competent care must be emphasized within healthcare systems to ensure that providers recognize and actively address the unique healthcare needs of diverse populations. By creating a more inclusive health system, we can work to level the playing field and reduce the discrepancies in maternal health outcomes.
Moreover, data collection on maternal health outcomes must be more transparent and comprehensive, allowing for more precise identification of risk factors affecting different racial and ethnic groups. Establishing a robust surveillance system to track these outcomes more effectively will not only reveal disparities but also inform targeted interventions tailored to those at highest risk.
Engagement with diverse communities is also essential to enhance trust between expectant mothers and healthcare providers. By fostering relationships and ensuring open lines of communication, healthcare systems can better address and navigate the barriers that disproportionately affect women of color, thus working towards equitable maternal health for all.
Improving Postpartum Care for Better Maternal Health
Postpartum care is a critical, yet often underestimated, component of maternal health that requires urgent improvements. The recognition that nearly a third of maternal deaths occur after the 42-day postpartum period signals the need for a reevaluation of healthcare models that support new mothers. Many current practices treat postpartum recovery as a six-week event, failing to acknowledge the continuous healthcare needs of women post-delivery.
Improving postpartum care could entail extending healthcare services past the traditional check-up timeframe, including regular mental and physical health assessments. Ensuring that new mothers receive comprehensive care that includes education about potential complications and continuous support can prevent avoidable tragedies. Integrating mental health resources into postpartum care frameworks is crucial, as mental health often significantly impacts overall maternal health outcomes.
Healthcare systems must prioritize educating new mothers about the signs of complications and encourage them to seek help when needed. Awareness campaigns can play a vital role in equipping women with information and resources that will help them navigate the postpartum period more effectively, ultimately reducing the risk of avoidable deaths.
Incorporating feedback from new mothers into care program designs can result in more effective and satisfying services. By addressing specific concerns that mothers face and tailoring solutions accordingly, healthcare systems can create a more supportive environment that prioritizes the long-term health and well-being of mothers during this crucial period.
Impact of Cardiovascular Disease on Pregnancy-Related Deaths
As recent studies show, cardiovascular disease has emerged as a leading cause of pregnancy-related deaths, surpassing other complications traditionally associated with childbirth. The transition from hemorrhage to cardiovascular disease reflects broader trends in public health, particularly the rising incidence of chronic conditions like hypertension among younger women. By understanding the connections between these health issues, we can better develop necessary interventions aimed at mitigating their impact during pregnancy.
Addressing cardiovascular health during the prenatal and postpartum periods involves not only clinical care but also lifestyle changes. Awareness initiatives that guide women on the importance of monitoring blood pressure and maintaining a healthy lifestyle during pregnancy can help reduce associated risks. Ensuring that healthcare providers are trained in recognizing the signs of cardiovascular distress can enhance early detection and preventative care.
Furthermore, understanding risk factors, such as obesity and diabetes, which contribute to cardiovascular issues, is vital in creating a healthier population of pregnant women. Supportive programs that encourage women to engage in healthier behaviors before, during, and after pregnancy can substantially reduce the risk of developing chronic conditions that lead to adverse maternal health outcomes.
Engaging in research that further explores the relationship between pre-existing conditions and pregnancy complications will also provide a wealth of information. Effective surveillance and tracking of these conditions in pregnancy can help refine treatment protocols and health education programs, ensuring a healthier journey for expectant mothers.
The Importance of Tracking Maternal Mortality
Tracking maternal mortality is essential for understanding the landscape of maternal health within the United States. For too long, the country lacked a consistent system for documenting pregnancy-related deaths, which has hindered efforts to analyze and address contributing factors effectively. With improved data collection through the implementation of pregnancy checkboxes on death certificates, we have begun to uncover the true scope of the challenge facing maternal health.
The ability to trace maternal deaths back to specific causes not only identifies trends but also informs targeted interventions. With a robust tracking system in place, healthcare policymakers and providers can focus their resources and attention on the most pressing issues, ensuring that preventable deaths are appropriately addressed. However, funding for these initiatives must be sustained and expanded to continue building on the progress made thus far.
The new findings surrounding late maternal deaths, as previously disregarded within traditional definitions, call for a broader understanding of maternal mortality. Recognizing that the challenges faced by new mothers extend beyond the immediate postpartum period sheds light on the need for continued support and effective health strategies during the first year of motherhood.
Investing in comprehensive data collection and analysis efforts is vital for improving maternal health outcomes. By actively tracking these statistics and connecting them with health policies, we can support informed decision-making that prioritizes the need for quality care and resources tailored to women’s health during and after pregnancy.
Future Directions in Maternal Health Research
The future of maternal health research must focus on identifying root causes of the alarming trends we currently observe in pregnancy-related deaths. Broadening the scope of research to include socio-economic factors, systemic barriers to care, and the long-term impacts of chronic health conditions will provide a better understanding of how these issues intersect. This comprehensive approach will pave the way for innovative solutions and effective health interventions.
Funding should be directed toward initiatives that promote research collaborations between academic institutions and community organizations. Engaging stakeholders at every level not only fosters improved understanding of the unique challenges faced by various demographics but also contributes to developing culturally relevant solutions. The voice of community members should be respected and integrated into research priorities, ensuring that the solutions generated are truly effective.
Moreover, advocacy for policies that address social determinants of health is crucial in shifting the maternal health landscape. Strategies that focus on improving access to healthcare, economic stability, and education for at-risk populations will help eliminate barriers that contribute to prevent measurable outcomes.
Ultimately, the journey toward improving maternal health outcomes requires sustained commitment across sectors, including healthcare, research, and community support. By prioritizing this issue and embedding it within broader public health strategies, we can work towards a future where maternal mortality rates are significantly reduced, benefiting mothers and children alike.
Frequently Asked Questions
What are the leading causes of pregnancy-related deaths in the U.S.?
In the U.S., cardiovascular disease has become the leading cause of pregnancy-related deaths, accounting for over 20% of such fatalities. This shift may be due to increasing rates of chronic conditions like hypertension among younger individuals, which necessitates comprehensive care during and after pregnancy.
Why is the U.S. maternal mortality rate so high compared to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, often attributed to a fragmented healthcare system, inequitable access to care, and persistent racial disparities in maternal health outcomes. Improving access to quality prenatal and postpartum care could significantly reduce preventable pregnancy deaths.
How do racial disparities affect the rates of pregnancy-related deaths?
Racial disparities critically affect maternal mortality, with American Indian and Alaska Native women experiencing the highest rates of pregnancy-related deaths. Such inequities highlight the urgent need for targeted public health interventions to improve outcomes for historically marginalized groups.
Are there significant differences in pregnancy-related death rates across states?
Yes, there is considerable variation in pregnancy-related death rates across states. Rates can range dramatically, underscoring the importance of addressing specific state-level policies and healthcare access to combat maternal mortality effectively.
What is being done to improve postpartum care in relation to preventable pregnancy deaths?
There is a growing recognition of the need to extend postpartum care beyond the traditional six-week checkup. Investing in continuous postpartum healthcare services is critical to reducing preventable pregnancy deaths and improving maternal health outcomes in the long run.
How does cardiovascular disease contribute to maternal mortality rates?
Cardiovascular disease now leads as a cause of pregnancy-related deaths, often resulting from conditions like hypertension and cardiac complications that can arise during pregnancy. Early recognition and management of these conditions are essential for reducing risk.
What are the implications of late maternal deaths for public health policies?
Late maternal deaths, occurring from 42 days to one year postpartum, account for a significant portion of pregnancy-related deaths. Acknowledging this period in public health policies can lead to improved healthcare strategies that support women during their transition into motherhood.
What measures can be taken to reduce racial disparities in maternal health?
To reduce racial disparities in maternal health, it is crucial to implement policies that address systemic inequities, enhance access to quality care for all women, and invest in community-based programs that cater to the unique needs of diverse populations.
How does improved tracking of pregnancy-related deaths help public health efforts?
Implementing a national system for tracking pregnancy-related deaths helps identify trends, disparities, and areas for improvement, which can inform health policies and interventions aimed at reducing maternal mortality rates effectively.
What role does chronic disease play in pregnancy-related deaths?
The rise in chronic diseases among younger populations, such as hypertension and cardiovascular conditions, has a direct impact on pregnancy-related mortality rates, necessitating proactive management and tailored healthcare interventions throughout pregnancy.
| Key Points |
|---|
| U.S. has highest maternal mortality among high-income countries |
| More than 80% of pregnancy-related deaths are preventable |
| Maternal mortality rates rose from 2018 to 2022; especially sharp in 2021 |
| Significant disparities exist by race and location |
| Cardiovascular diseases are leading causes of pregnancy-related deaths |
| Late maternal deaths (42 days to 1 year post-pregnancy) account for nearly a third |
| Need for improved prenatal and extended postpartum care |
Summary
Pregnancy-related deaths in the U.S. continue to rise, prompting serious concerns over maternal health. As the nation grapples with one of the highest maternal mortality rates among developed countries, the findings of recent studies underscore the urgent need for improved healthcare infrastructure. With significant disparities in maternal mortality rates influenced by race and geography, it is vital to address systemic inequities and enhance the quality of care available to pregnant individuals. Efforts must focus on ensuring accessible prenatal services and focusing on long-term postpartum recovery to mitigate these preventable deaths.